Something as vital and complex as the nervous system impacts nearly every medical specialty as well as cultural activities like politics, sports and arts.
This concept inspired the installation of our art exhibit Neurology, Illustrated, where each piece provides insight into neurology in society. Directly or indirectly, artists have depicted the effects of neurological disorders for thousands of years, while for others, their own neurological conditions impacted the art they produced.
Yet, our interests extend far beyond art curation. Through our clinical trials, research initiatives and training programs, we continuously expand our expertise on the system responsible for our thoughts, movements and emotions.
Neurology, Illustrated at Tufts Medical Center
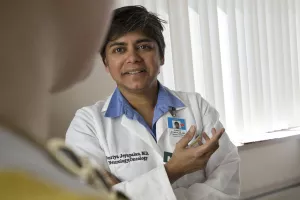
David Thaler, MD, PhD, FAHA, Neurologist-in-Chief at Tufts Medical Center, proudly displays the department's art exhibit, Neurology, Illustrated, complete with pieces that provide insight into neurology in society.